The Critical Differences: Pathogenicity & Virulence
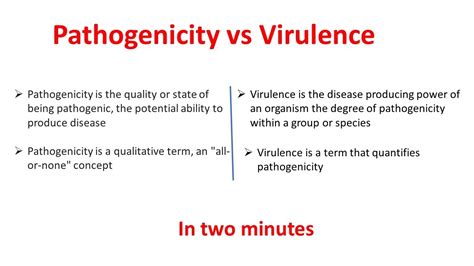
The terms "pathogenicity" and "virulence" are often used interchangeably when discussing infectious agents, such as bacteria, viruses, or fungi. While these concepts are closely related and interconnected, there are subtle yet critical differences that distinguish them. Understanding these differences is essential for healthcare professionals, researchers, and students alike, as it provides a deeper insight into the complex world of infectious diseases and their management.
In this article, we delve into the intricacies of pathogenicity and virulence, exploring their definitions, mechanisms, and the factors that influence them. By the end of this exploration, you will gain a comprehensive understanding of these fundamental concepts and their implications in the realm of infectious diseases.
Pathogenicity: The Ability to Cause Disease
Pathogenicity refers to the inherent capacity of a microorganism to cause disease in a susceptible host. It is a fundamental characteristic of many pathogens, determining their potential to initiate an infectious process. Pathogenicity is not solely dependent on the pathogen itself but is influenced by a multitude of factors, including the host's immune status, environmental conditions, and the specific traits of the pathogen.
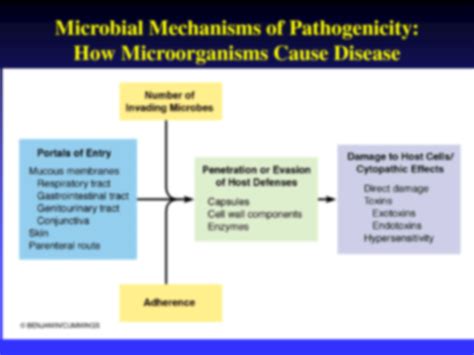
Mechanisms of Pathogenicity
Pathogens employ various strategies to establish an infection within a host. These mechanisms can be broadly categorized as follows:
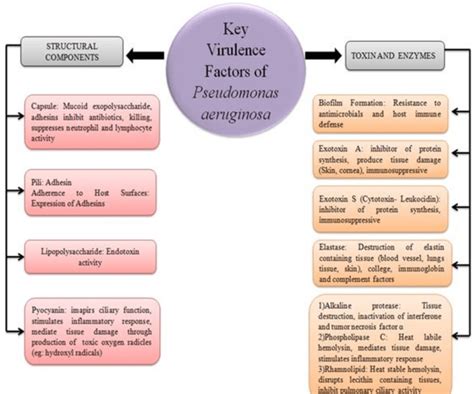
- Adhesion and Invasion: Pathogens often possess specific structures, such as fimbriae or pili, that enable them to attach to host cells. This adhesion is a crucial step in initiating infection. Once attached, some pathogens invade the host cells, establishing an intracellular niche, while others remain extracellular.
- Evading Host Defenses: Pathogens have evolved mechanisms to evade or subvert the host's immune system. This can involve disguising themselves through antigenic variation or producing immune-modulating molecules that suppress the host's immune response.
- Toxins and Virulence Factors: Many pathogens produce toxins or other virulence factors that directly contribute to disease. These factors can damage host cells, disrupt physiological processes, or facilitate pathogen replication and spread.
- Nutrient Acquisition: Pathogens compete with the host for essential nutrients. Some pathogens have evolved strategies to acquire nutrients more efficiently, such as through the production of enzymes that break down complex molecules into usable forms.
The specific mechanisms employed by a pathogen can vary greatly depending on its taxonomic group and the host it infects. For example, the bacterium Salmonella uses a type III secretion system to inject effector proteins into host cells, disrupting cellular processes and facilitating its own survival and replication.
Factors Influencing Pathogenicity
The pathogenicity of a microorganism is influenced by a complex interplay of factors, including:
- Host Susceptibility: The susceptibility of a host to a particular pathogen can vary based on age, immune status, genetic factors, and overall health. For instance, individuals with compromised immune systems, such as those with HIV/AIDS, are more susceptible to opportunistic infections.
- Pathogen Dose: The dose or concentration of the pathogen can impact its pathogenicity. Higher doses may lead to more severe disease, as seen in cases of foodborne illness caused by high concentrations of Salmonella bacteria.
- Environmental Conditions: Environmental factors, such as temperature, humidity, and pH, can affect the survival and growth of pathogens. For example, Legionella bacteria thrive in warm, aqueous environments, making them a concern in poorly maintained water systems.
- Pathogen-Host Interaction: The specific interaction between the pathogen and the host can influence the disease outcome. Some pathogens may have a broader host range, while others are highly specialized, infecting only a specific host species or tissue type.
Understanding these factors is crucial for developing effective strategies to prevent and control infectious diseases. For instance, implementing strict food safety measures can help reduce the dose of pathogens, thereby decreasing the risk of disease.
Virulence: The Measure of Disease Severity
Virulence, on the other hand, refers to the degree of pathogenicity or the severity of the disease caused by a microorganism. It is a quantitative measure that assesses the ability of a pathogen to produce harm or damage to the host. Virulence is often associated with the concept of "fitness," indicating the success of a pathogen in establishing an infection and transmitting to new hosts.
Factors Affecting Virulence
The virulence of a pathogen is influenced by a combination of intrinsic and extrinsic factors. Intrinsic factors are inherent properties of the pathogen, while extrinsic factors relate to the host and the environment.
| Intrinsic Factors | Extrinsic Factors |
|---|---|
| Genetic Makeup | Host Immune Response |
| Toxin Production | Nutritional Status of Host |
| Growth Rate | Environmental Stressors |
| Mode of Transmission | Co-Infections |
For instance, the Escherichia coli strain O157:H7 is highly virulent due to its ability to produce a potent toxin called Shiga toxin. This toxin can cause severe damage to the host's kidneys and gastrointestinal tract, leading to a potentially fatal condition known as hemolytic uremic syndrome.
Quantifying Virulence
Virulence can be quantified using various methods, including:
- Median Lethal Dose (LD50): This measures the dose of a pathogen required to kill 50% of the infected hosts. A lower LD50 indicates higher virulence.
- Median Infectious Dose (ID50): Similar to LD50, ID50 represents the dose of a pathogen required to infect 50% of susceptible hosts.
- Disease Severity Scoring: Researchers can assign scores to various disease symptoms or outcomes, allowing for a quantitative assessment of virulence.
- Genetic Studies: Advances in genomics have enabled researchers to identify and study virulence genes, providing insights into the molecular basis of virulence.
By quantifying virulence, scientists can compare the disease-causing potential of different pathogens, assess the impact of genetic mutations, and develop targeted interventions to mitigate the severity of infectious diseases.
The Interplay between Pathogenicity and Virulence
Pathogenicity and virulence are interconnected concepts that shape the dynamics of infectious diseases. While pathogenicity determines the ability of a pathogen to cause disease, virulence quantifies the severity of that disease. A pathogen with high pathogenicity may not necessarily be highly virulent, and vice versa.
Consider the example of Mycobacterium tuberculosis, the causative agent of tuberculosis (TB). While M. tuberculosis is highly pathogenic, not all individuals infected with the bacterium develop active TB. The virulence of M. tuberculosis is influenced by factors such as the host's immune status and the specific strain of the bacterium. Some strains are more virulent than others, leading to more severe disease.
Implications for Public Health and Clinical Practice
Understanding the concepts of pathogenicity and virulence has far-reaching implications for public health and clinical practice. It informs the development of effective prevention strategies, such as vaccines and antimicrobial therapies, and guides the management of infectious diseases.
Vaccine Development
Vaccines are designed to induce an immune response against specific pathogens. By understanding the pathogenicity and virulence of a pathogen, researchers can identify the most appropriate antigens to include in a vaccine, ensuring a robust and specific immune response.
Antimicrobial Resistance
The increasing prevalence of antimicrobial resistance is a global health concern. By studying the virulence factors and mechanisms of pathogens, researchers can develop targeted therapies that disrupt these factors, potentially overcoming resistance and improving treatment outcomes.
Infectious Disease Surveillance
Surveillance programs play a critical role in monitoring and controlling infectious diseases. By quantifying the virulence of pathogens, public health officials can identify emerging threats, track disease trends, and implement targeted interventions to prevent and control outbreaks.
Conclusion
In conclusion, the concepts of pathogenicity and virulence provide a lens through which we can understand and manage infectious diseases. While pathogenicity defines the ability of a pathogen to cause disease, virulence quantifies the severity of that disease. By exploring these concepts and their underlying mechanisms, we gain insights into the complex world of infectious agents and their interactions with hosts.
As our understanding of pathogenicity and virulence continues to evolve, so too will our ability to prevent, control, and treat infectious diseases. The ongoing research in this field holds promise for a healthier future, where the impact of infectious diseases is minimized through targeted interventions and effective public health measures.
How do pathogens cause disease in the first place?
+Pathogens cause disease through various mechanisms, including adhesion and invasion of host cells, evasion of host immune responses, and production of toxins or virulence factors. These factors can disrupt normal physiological processes, leading to disease symptoms.
Can a pathogen be pathogenic but not virulent?
+Yes, a pathogen can possess the ability to cause disease (pathogenicity) but may not produce severe symptoms or damage to the host (low virulence). This is often seen in asymptomatic infections or when the host’s immune system effectively controls the pathogen.
How do we measure the virulence of a pathogen?
+Virulence can be quantified using various methods, including median lethal dose (LD50), median infectious dose (ID50), disease severity scoring, and genetic studies to identify virulence genes.