Understanding Nurses' Notes: 5 Essentials
In the intricate world of healthcare documentation, nurses' notes serve as a vital record of patient care and play a crucial role in ensuring continuity and quality of treatment. These notes are a comprehensive account of a patient's medical journey, providing insights into their condition, treatment progress, and the care provided by nursing staff. Understanding the essentials of nurses' notes is key to appreciating their significance and the impact they have on patient care and outcomes.
The Art and Science of Nurses' Notes

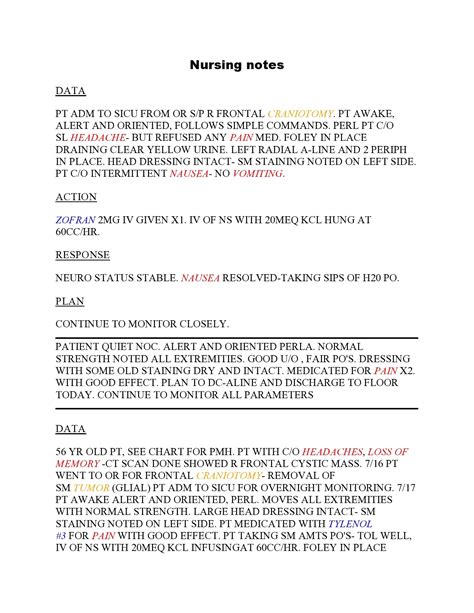
Nurses' notes are a meticulous record of a patient's daily experience within a healthcare setting. They document the patient's vital signs, treatment plans, medication administration, and any significant observations or changes in their condition. These notes are a blend of art and science, requiring nurses to combine their clinical expertise with a precise and concise writing style.
1. Accuracy and Precision
The foundation of effective nurses' notes lies in their accuracy and precision. Nurses must record information as accurately as possible, ensuring that their notes reflect the true status of the patient's health. This includes capturing all relevant details, such as the patient's response to treatment, any adverse reactions, and the timing of medication administration. By maintaining high standards of accuracy, nurses ensure that their notes provide an honest and comprehensive account of the patient's journey.
| Metric | Importance |
|---|---|
| Vital Sign Accuracy | Critical for patient monitoring and treatment planning. |
| Medication Documentation | Ensures patient safety and adherence to treatment plans. |
| Observational Notes | Captures patient progress and potential complications. |

2. Consistency and Standardization
Consistency is another key aspect of nurses' notes. Healthcare institutions often have standardized formats and guidelines for nursing documentation to ensure uniformity and ease of understanding. Standardized notes make it simpler for different healthcare professionals to interpret and act upon the information, fostering a collaborative environment.
For instance, many institutions use the SOAPIE format, which stands for Subjective, Objective, Assessment, Plan, Implementation, and Evaluation. This format provides a structured approach to documenting a patient's progress, ensuring that all vital information is captured.
3. Timeliness and Promptness
Nurses' notes should be made promptly, ideally as soon as possible after an event or observation. Timely documentation ensures that the details are fresh in the nurse's mind, leading to more accurate and reliable records. Prompt note-taking also facilitates immediate communication among the healthcare team, allowing for quick responses to any emerging patient needs.
4. Clear and Concise Communication
Effective nurses' notes are characterized by clear and concise language. Nurses should strive to communicate complex medical information in a straightforward manner, ensuring that their notes are easily understood by all members of the healthcare team. This clarity is crucial for effective collaboration and patient care.
For example, instead of writing "The patient exhibited signs of distress," a more precise and concise note might read, "Patient displayed increased heart rate and blood pressure, indicating potential anxiety or pain."
5. Ethical and Legal Considerations
Nurses' notes carry significant ethical and legal weight. They serve as a legal record of the care provided and can be used as evidence in various healthcare-related matters. Therefore, nurses must maintain strict confidentiality and ensure that their notes do not contain any sensitive information that could be misused or misunderstood.
Furthermore, nurses should be aware of the potential implications of their notes and how they could impact patient care and healthcare decisions. Accurate and responsible documentation is a cornerstone of ethical nursing practice.
The Impact of Nurses' Notes
The role of nurses' notes extends far beyond mere documentation. They are a powerful tool for improving patient care, facilitating collaboration among healthcare professionals, and enhancing the overall quality of healthcare services.
Enhancing Patient Care
Nurses' notes provide a detailed account of a patient's medical journey, offering insights into their progress and any challenges they may face. This information is invaluable for tailoring treatment plans to the individual needs of each patient. By carefully documenting responses to treatment, nurses can help identify what works best for each patient, leading to more effective and personalized care.
Facilitating Interprofessional Collaboration
In today's healthcare landscape, collaboration among various professionals is essential for providing holistic patient care. Nurses' notes serve as a common language, allowing different healthcare providers to understand the patient's condition and the care provided. This shared understanding fosters effective teamwork and ensures that patients receive consistent and coordinated care.
Improving Healthcare Quality
The data captured in nurses' notes can be used to improve the quality of healthcare services. By analyzing patterns and trends in patient care, healthcare institutions can identify areas for improvement, such as optimizing medication administration practices or enhancing pain management strategies. This data-driven approach to quality improvement is made possible by the detailed and accurate documentation provided by nurses.
Legal and Ethical Implications
Nurses' notes also have significant legal and ethical implications. They provide a clear record of the care provided, which can be crucial in legal proceedings or ethical inquiries. Accurate and responsible documentation can protect both patients and healthcare professionals, ensuring that the rights and welfare of all parties are respected.
The Future of Nurses' Notes
As healthcare technology advances, the landscape of nurses' notes is also evolving. Electronic Health Records (EHRs) are becoming increasingly prevalent, offering more efficient and accessible methods of documentation. EHRs allow for real-time updates, seamless sharing of information, and the potential for advanced data analysis.
However, with the transition to digital documentation, nurses must adapt to new challenges. These include ensuring data security, maintaining accurate and up-to-date records, and adapting to the specific functionalities of the EHR system. Despite these challenges, the benefits of EHRs in terms of improved access, efficiency, and data analysis capabilities are significant.
Adapting to Technological Advances
Nurses will need to continuously update their skills to effectively utilize EHRs and other emerging technologies. This may include training in data security, privacy protocols, and the efficient use of digital documentation tools. By embracing these technologies, nurses can further enhance the quality and efficiency of their documentation, ultimately improving patient care.
Conclusion
Nurses' notes are a vital component of patient care and healthcare documentation. They reflect the dedication, expertise, and ethical commitment of nursing professionals. By understanding and embracing the essentials of nurses' notes, we can appreciate their role in improving patient outcomes, facilitating collaboration, and advancing the quality of healthcare services.
Frequently Asked Questions
How often should nurses update their notes?
+Nurses should update their notes as soon as possible after a significant event or observation. Prompt documentation ensures accuracy and facilitates timely communication among the healthcare team. In general, notes should be updated at least once per shift, but more frequently if there are notable changes in the patient's condition.
<div class="faq-item">
<div class="faq-question">
<h3>What are some common challenges in nurses' note-taking?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Common challenges include maintaining accuracy and precision, especially when dealing with complex medical conditions. Nurses must also balance the need for thorough documentation with the demand for timeliness. Additionally, adapting to new documentation technologies, such as EHRs, can present learning curves and require ongoing training.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>How do nurses' notes contribute to patient safety?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Nurses' notes play a critical role in patient safety by providing a detailed record of the patient's condition and the care provided. This information helps healthcare professionals make informed decisions, identify potential risks or complications, and ensure that patients receive the right treatment at the right time. Accurate and timely documentation can prevent errors and improve patient outcomes.</p>
</div>
</div>
</div>