Alpha Beta Gamma Hemolysis
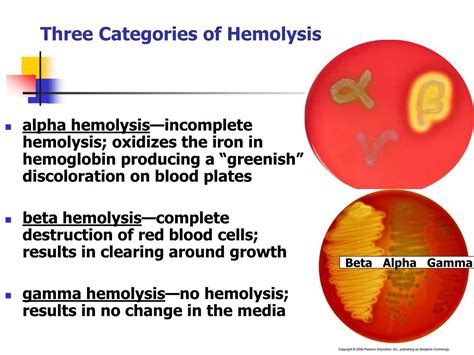
Understanding Alpha, Beta, and Gamma Hemolysis: A Comprehensive Guide
Hemolysis, the breakdown of red blood cells, is a critical process in microbiology, especially when identifying bacteria through various tests. Among these tests, hemolysis plays a vital role in distinguishing bacterial species, as it indicates how these microorganisms interact with red blood cells. This article will delve into the intricacies of Alpha, Beta, and Gamma hemolysis, shedding light on their unique characteristics, mechanisms, and applications in the field of microbiology.
The Fundamentals of Hemolysis
Hemolysis is a complex process involving the rupture of red blood cells (RBCs), resulting in the release of their contents, primarily hemoglobin. This breakdown can occur due to various factors, including physical or chemical stressors, as well as the presence of specific bacterial species. The study of hemolysis provides valuable insights into the behavior of bacteria and their potential impact on the human body.
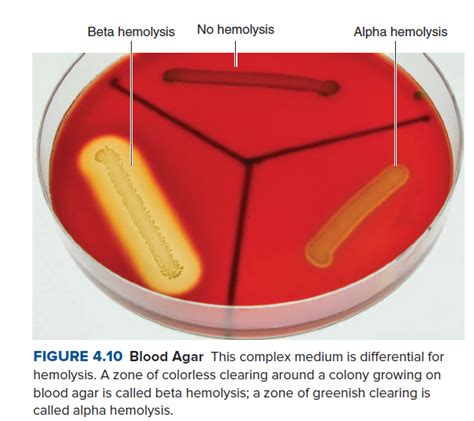
In the context of bacterial identification, hemolysis tests are performed on blood agar plates, a type of growth medium infused with sheep or horse blood. When bacteria are cultured on these plates, their interaction with the red blood cells leads to distinct patterns of hemolysis, which serve as crucial indicators for classification.
Unraveling Alpha Hemolysis
Alpha hemolysis, also known as partial or incomplete hemolysis, is characterized by a greenish discoloration surrounding the bacterial growth on the blood agar plate. This unique color change is attributed to the oxidation of hemoglobin, resulting in the formation of green bile pigments. Alpha-hemolytic bacteria possess the ability to partially lyse red blood cells, leading to this distinctive appearance.
Key Features of Alpha Hemolysis
- Greenish zone around bacterial colonies
- Indication of incomplete hemolysis
- Oxidation of hemoglobin to green bile pigments
- Commonly observed in bacteria like Streptococcus pneumoniae and certain species of Neisseria
The mechanism behind alpha hemolysis involves the production of hydrogen peroxide (H2O2) by the bacteria, which can diffuse into the surrounding medium. This hydrogen peroxide then interacts with the hemoglobin in the red blood cells, leading to its oxidation and the formation of the characteristic green discoloration.
| Alpha-Hemolytic Bacteria | Examples |
|---|---|
| Streptococcus pneumoniae | A common cause of pneumonia and meningitis |
| Neisseria sicca | A species found in the oral cavity and upper respiratory tract |
| Neisseria mucosa | A normal flora of the mouth and nasopharynx |
Exploring Beta Hemolysis
Beta hemolysis, also referred to as complete or clear hemolysis, is characterized by a clear zone surrounding the bacterial growth on the blood agar plate. This indicates a complete breakdown of red blood cells, resulting in the release of their contents into the surrounding medium. Beta-hemolytic bacteria possess powerful enzymes and toxins that can lyse red blood cells effectively.
Distinctive Traits of Beta Hemolysis
- Clear zone around bacterial colonies
- Indication of complete hemolysis
- Release of hemoglobin and other cell contents
- Commonly observed in pathogenic bacteria like Streptococcus pyogenes and certain Clostridium species
The mechanism of beta hemolysis involves the production of powerful enzymes, such as streptolysin O and streptolysin S, by the bacteria. These enzymes can directly lyse red blood cells, leading to the release of hemoglobin and other cellular components. Additionally, some beta-hemolytic bacteria produce toxins that can cause lysis of red blood cells through different pathways.
| Beta-Hemolytic Bacteria | Examples |
|---|---|
| Streptococcus pyogenes | A major cause of strep throat and rheumatic fever |
| Clostridium perfringens | A common cause of gas gangrene |
| Clostridium tetani | The causative agent of tetanus |
Unveiling Gamma Hemolysis
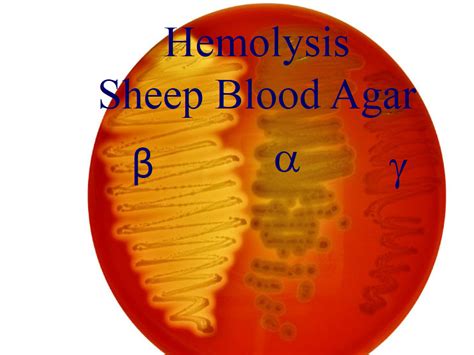
Gamma hemolysis, also known as non-hemolytic or non-hemolysis, is the absence of any hemolytic activity by the bacteria on the blood agar plate. This means that the bacteria do not interact with the red blood cells, resulting in no visible changes to the agar surrounding the bacterial growth.
Characteristics of Gamma Hemolysis
- No visible changes to the agar
- Indication of no hemolytic activity
- Commonly observed in bacteria like Staphylococcus epidermidis and certain non-pathogenic species
The absence of hemolysis in gamma-hemolytic bacteria can be attributed to their lack of enzymes or toxins that can lyse red blood cells. These bacteria coexist with red blood cells without causing any harm or breakdown.
| Gamma-Hemolytic Bacteria | Examples |
|---|---|
| Staphylococcus epidermidis | A common skin flora that can cause infections in immunocompromised individuals |
| Lactobacillus species | Normal flora of the gastrointestinal tract and vagina |
| Corynebacterium species | Normal flora of the skin and mucous membranes |
Applications and Clinical Significance
The understanding of Alpha, Beta, and Gamma hemolysis has significant implications in clinical microbiology. By interpreting hemolytic patterns, microbiologists can identify and differentiate between various bacterial species, aiding in the diagnosis and treatment of infections. Additionally, the hemolytic activity of bacteria provides valuable insights into their pathogenic potential and virulence mechanisms.
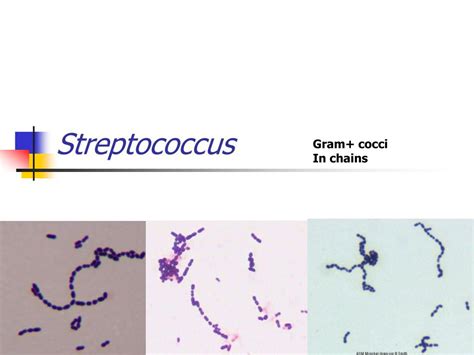
Hemolysis tests are particularly crucial in identifying and classifying streptococcal species, as they exhibit diverse hemolytic patterns. For instance, the differentiation between alpha-hemolytic Streptococcus pneumoniae and beta-hemolytic Streptococcus pyogenes is essential in diagnosing and treating pneumonia versus streptococcal pharyngitis.
Future Perspectives
As our knowledge of microbiology expands, further research into the mechanisms and implications of hemolysis will undoubtedly uncover new insights. Advanced techniques, such as molecular biology and genomic analysis, may provide a deeper understanding of the genes and pathways involved in hemolytic activity. Additionally, the exploration of hemolysis in other microbial species beyond bacteria could open new avenues of research.
The study of hemolysis remains an essential tool in the field of microbiology, contributing to our understanding of bacterial behavior and its impact on human health. As we continue to unravel the complexities of hemolysis, we move closer to developing more effective diagnostic and therapeutic strategies.
How is Alpha Hemolysis different from Beta Hemolysis?
+Alpha hemolysis is characterized by a greenish discoloration around the bacterial growth, indicating partial hemolysis. In contrast, beta hemolysis results in a clear zone, signifying complete hemolysis and the breakdown of red blood cells.
What are the clinical implications of Gamma Hemolysis?
+Gamma hemolysis indicates the absence of hemolytic activity, which may suggest a less virulent or non-pathogenic nature of the bacteria. However, it’s important to note that some gamma-hemolytic bacteria can still cause infections, especially in immunocompromised individuals.
Can hemolysis patterns change in different growth conditions?
+Yes, hemolysis patterns can vary depending on the growth conditions, such as temperature, pH, and the presence of specific nutrients. Some bacteria may exhibit different hemolytic activities under different environmental conditions.



